Parents' guide to sore throats
About the author: Sophie is a General Practitioner who has previously worked with Night Doctor and now based in the South West, WA. She has an interest in women’s and children’s health and has completed additional training in obstetrics and gynaecology, sexual health and skin cancer surgery. Aside from her clinical work she also teaches medical students at the University of Notre Dame, was formerly a co-opted member of the RACGP WA Faculty Board, and is a current delegate for the RACGP Future Leaders Program.
Artist: @ellieloomes
Sore throats and tonsillitis are a common childhood illness seen in general practice and by after-hours services such as Night Doctor. There is often confusion around the cause of a throat infection and whether it requires antibiotics. In this blog we answer the most common questions we get asked by parents about sore throats.
What causes a sore throat in children?
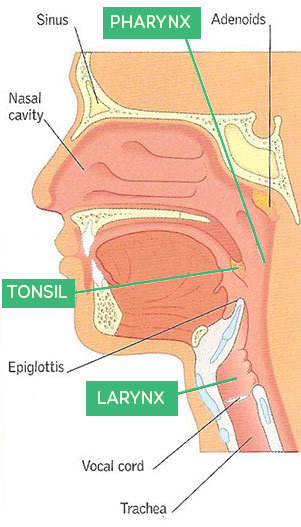
The most common cause of an acute sore throat in children is a viral infection, such as the common cold virus. Other viral infections, such as glandular fever, and bacterial infections can also cause sore throats, but these are less common.1.5 There are different areas of the throat that can be affected by a viral or bacterial infection, such as the pharynx, larynx or tonsils (see diagram below). The tonsils are part of the body’s natural immune system and they help to prevent infections, however they can also become infected by either a virus or bacteria, causing tonsillitis.2
How do I know if my child has a throat infection?
Your child may have a throat infection if they are saying that they have a sore throat. Other symptoms of a throat infection may be neck pain, painful swallowing, fever, drooling, loss of appetite or a change in the sound of their voice. Sometimes younger children may not complain of a sore throat, and may have other symptoms such as tummy pain or vomiting. Very young children may just have a fever and no other symptoms.2
What can I do to help their sore throat?
If your child has a sore throat, they may not have much appetite for a day or two. It is important to offer your child small amounts of fluid often until they are eating again. Some children may prefer to suck on an icy-pole or have a warm drink. It may also help to offer them soft, cool foods such as jelly or ice-cream, which may soothe the throat as they eat them.2,3,4
If you think additional pain relief is required, you can give your child simple pain killers such as paracetamol or ibuprofen, at the correct dosing for their age/weight. There are many products available at pharmacies, such as lozenges, sprays and gargles that have antiseptic and/or numbing effects, however there is little evidence that these offer any more benefit than just paracetamol or ibuprofen.1
Should my child see a doctor if they have a sore throat?
If your child has a sore throat, or any of the symptoms mentioned above, it is not unreasonable to see a doctor to get their throat checked. You should not delay seeking medical attention if your child has a sore throat and:
-
Has trouble breathing or swallowing
-
Is drooling more than usual
-
Has a stiff or swollen neck
-
Has a fever for no apparent reason
-
Is not drinking enough fluid
-
Has a rash
-
Seems very sick or you are worried for any other reason
Does my child need antibiotics?
This is the most common question we get asked about sore throats. It can be confusing for parents because some sore throats are given antibiotics and others are not. Only throat infections that are caused by bacteria require antibiotics, and if the cause is a virus antibiotics will not help.2,5
Often it is clear when a throat infection is caused by bacteria, however sometimes looking at the throat or tonsils does not clearly tell us whether it is caused by a virus or bacteria.2 As doctors we may look for certain criteria which make a bacterial infection more likely (such as their age, whether there is pus on the throat/tonsils, swollen and tender lymph nodes (or ‘glands’) in the neck, a high fever, and whether or not they have a cough).6 However even in children who do have some of these criteria, most will get better within a week regardless of whether they take antibiotics.2,4 Your doctor may discuss with you how likely it is that your child has a bacterial throat infection, and the risks and benefits of deciding to start antibiotics.
Certain children are more at risk of complications from throat infections, and may be more likely to be given antibiotics to help prevent these complications. This includes children of Aboriginal or Torres Strait Islander background, children who have weakened immune systems, children who have a rash that may be Scarlet Fever, or children who have had acute rheumatic fever in the past.6,7
Scarlet fever
Scarlet fever is a streptococcal bacterial infection that often causes a sore throat and commonly has the following signs and symptoms8:
- Fever
- Swollen tonsils and neck glands
- A fine red rash (typically develops 12 to 24 hours after symptoms begin and lasts 2 to 5 days)
- A very red (strawberry-like) tongue
- Headaches
- Nausea and vomiting
Scarlet fever requires antibiotic treatment. If you child has a sore throat or any of the above symptoms you should seek a prompt medical review.
Why does my child keep having throat infections, and do they need their tonsils removed?
Recurrent sore throats are common in children, and this is because the common cold viruses which cause most sore throats are very common in children.1 Some children may have recurrent attacks of tonsillitis, however these usually become less frequent as they grow older and their defences against infection become fully developed. Surgery is only needed if a child has many attacks in a year, or has problems with breathing or snoring because of their large tonsils.2 If you are worried about your child having recurrent attacks of sore throat or tonsillitis, you should discuss this with your GP.
References
- Australian Medicines Handbook, 2018. Mouth and Throat Conditions.
- Better Health Channel, 2017. Streptococcal infection - group A.
- Health Direct, 2017. Strep throat self care.
- NPS Medicine Wise, 2017. Respiratory tract infections (RTIs) - nose, throat and lungs.
- Raising Children Network Australia, 2015. Health Reference: Sore Throat.
- Therapeutic Guidelines, 2018. Acute pharyngitis and/or tonsillitis.
- The Royal Children’s Hospital Melbourne, 2018. Clinical Practice Guideline: Sore Throat.
- Health WA, 2018. Scarlet Fever
This information is general and may not apply to you or another person. If you have any concerns about your health or the health and wellbeing of a child, consult a doctor or other healthcare professional. You should never delay seeking medical advice, disregard medical advice, or discontinue medical treatment because of information on this website.
← Back to blog
