Parents’ guide to gastro
About the author: Sophie is a General Practitioner who has previously worked with Night Doctor and now based in the South West, WA. She has an interest in women’s and children’s health and has completed additional training in obstetrics and gynaecology, sexual health and skin cancer surgery. Aside from her clinical work she also teaches medical students at the University of Notre Dame, was formerly a co-opted member of the RACGP WA Faculty Board, and is a current delegate for the RACGP Future Leaders Program.
Artist: @ellieloomes
Gastroenteritis (more commonly referred to as ‘gastro’) is an illness that affects the gut and is characterised by diarrhoea and vomiting.4,7 It is often accompanied by fever, cramping abdominal pain and loss of appetite. Gastro is a common illness in children that is easily spread between people, and is a frequent reason for presentation to general practice, emergency departments, and after hours home visit services such as Night Doctor.3,5
The main aim of treatment is to replace the fluid lost through vomiting and diarrhoea. This will not stop the vomiting and diarrhoea but it will prevent your child from becoming dehydrated.7,11 Fortunately, most cases of gastro can be managed at home and only a small number of children require treatment in hospital.5,7
What causes gastro?
Most cases of gastro (about 70%) are caused by viruses, the most common being Rotavirus.4,11 Less commonly, it may also be caused by bacteria and parasites, which can occur from undercooked meats, unwashed fruits and salads, and contaminated water.3
I think my child has food poisoning - is that the same as gastro?
Food poisoning, sometimes referred to as ‘food-borne illness’, can occur from food contaminated with bacteria. It causes gastroenteritis symptoms that usually commence within 24-72 hours of eating the contaminated food. If you suspect your child’s gastro is caused by food poisoning, it is important to seek medical attention as they may require stool sample tests or treatment.13
How dehydrated is my child?
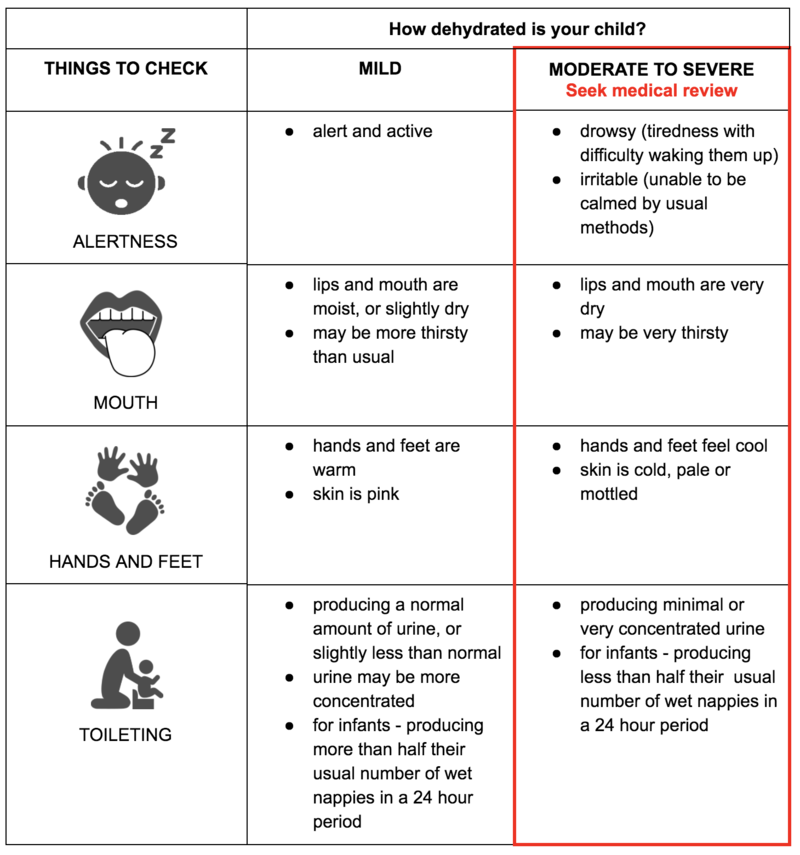 9,8,5
9,8,5
Most children with mild dehydration are appropriate for treatment at home. If your child has any features of moderate to severe dehydration, you should seek urgent review by a doctor.
What can I give my child to drink?
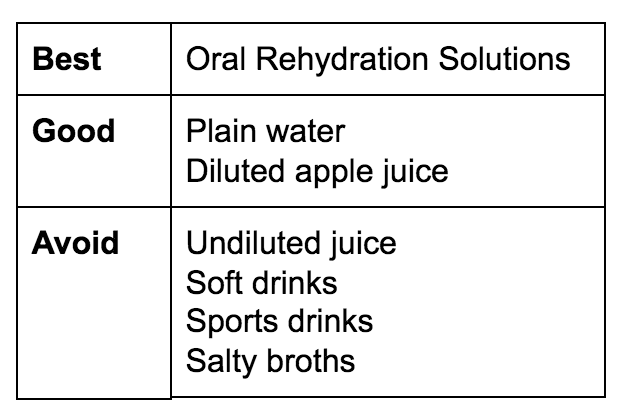
Most children with mild dehydration can be treated with oral fluid. The best fluids to give are Oral Rehydration Solutions (such as HYDRAlyte or Gastrolyte), as these contain the glucose and salts which are lost through vomiting and diarrhoea.4 If you do not have these, plain water or diluted apple juice (1 cup of unsweetened apple juice per 4 cups of water) may be given.5,10,11
Do not give undiluted juice, soft drinks or sports drinks, as they contain too much sugar, which can make diarrhoea and dehydration worse. For similar reasons, do not give salty liquids such as chicken broth.3,4
It is best to give small amounts of fluid frequently (every 15 minutes), as it is better tolerated than giving large volumes at a time. You can use a rehydration chart such as the Night Doctor Oral Rehydration Chart to ensure your child is getting an adequate amount of fluid for their size. Even if your child continues to vomit, still continue to offer sips of fluid, as some will still be retained and provide some hydration.11 If your child is refusing to drink, you can try offering an iceblock (e.g. Gastrolyte / HYDRAlyte Ice Blocks) .4,7
Breastfed infants
Breastfed infants should continue to be given breast milk, however they will likely need to be fed more frequently, and may also require supplementation with Oral Rehydration Solution or boiled water (subsequently cooled to room temperature before giving).4,11
Formula fed infants
There is differing opinion about what fluid to give formula fed infants. Some experts will recommend Oral Rehydration Solutions while there is significant vomiting, whereas others recommend continuing formula if your child is tolerating it.
The guidelines from our local children’s hospital, Princess Margaret Hospital for Children, say that it is safe to give formula while your child has gastro.9 However, if you find it is making the vomiting worse, you can try Oral Rehydration Solution while the vomiting is frequent, with the aim of re-introducing formula feeds within 24 hours. It is important to follow the preparation instructions for your particular formula and not to dilute the mixture, as this can cause your child to become very ill.4,11
Should I let my child eat?
It is no longer recommended to restrict food intake while your child has gastro, although it is normal for them to have a reduced appetite, particularly in the first 24 hours of the illness.4 You can continue to offer their normal foods and allow them to eat once they feel hungry again.3 Restarting a normal diet with balanced nutrients as soon as possible will help your child get better quicker.11
Temporary lactose intolerance may occur after an episode of gastro. It may be suspected if the diarrhoea becomes worse, or is frothy and explosive after consuming lactose-containing food/drinks such as milk or formula.11 It is important you see a doctor before restricting lactose intake in your child.
Should my child be given medicine to stop the diarrhoea and vomiting?
Medicines to stop vomiting may occasionally be given by doctors to children with persistent vomiting and dehydration, to help them with tolerating oral fluids. A commonly used medication to stop vomiting called Ondansetron is available in wafer form and has shown to be safe in children older than 6 months of age.5,9
Medicines to reduce diarrhoea are often not required. Routine use is not recommended. They do not improve dehydration significantly, and, like all medicines, they have potential side effects that can cause harm to your child.3
What about antibiotics or probiotics?
Antibiotic treatment is usually not required as most cases of gastro are caused by viruses.4 They may occasionally be given if a doctor suspects a bacterial cause of gastro.
There is some evidence that probiotics can decrease the duration of viral gastro, however there is a lack of research about the optimal type of probiotic, dosage and frequency. For this reason, their use is not currently recommended routinely.1
When can I expect my child to get better?
Gastro is usually a short-lived illness and most children recover quickly. Vomiting is often the first symptom to appear and can last for 2-3 days. The diarrhoea may persist longer, up to 10 days in some children.4, 5, 11, 12
If your child’s symptoms are lasting longer than expected (vomiting for more than 48 hours or diarrhoea longer than 10 days), you should seek medical attention even if your child is otherwise appearing well.4,11,12 If your doctor suspects that your child’s symptoms are caused by something other than a virus, they may do some tests such as a stool sample.4
When should I see a doctor?
You should not delay seeking medical attention if your child:
-
Is very young or very small (less than 6 months of age or less than 8kg weight)
-
Was born pre-term or has other health problems
-
Is vomiting blood or has blood or mucous in their diarrhoea
-
Is vomiting bile (dark green vomit)
-
Is in significant pain or has a tummy that is tender to press
-
Is not taking in enough fluids, or making less wet nappies than usual
-
Appears very tired or drowsy
-
Appears pale, or has mottled or blotchy skin
-
Has high fevers (>38.5 degrees)
-
Does not seem to be getting better, or you are worried for any other reason
3,4,9,11,12
Is it infectious? How do I stop it spreading to other family members?
Gastro is easily spread by contact with another person who has the illness,4,7,11 so good hygiene is important to prevent spread to other people, particularly those who are vulnerable such as infants, the elderly, pregnant women, and those with other health problems.
Handwashing, especially before preparing food, after changing nappies or handling your sick child, will help minimise the risk of spread.3,11,12 Alcohol-based hand sanitisers are more effective at removing bacteria and viruses from unsoiled hands than simple handwashing with soap and water.2,6 You should also ensure you wipe any toys that may be shared between your children.11
When can I return to work or my child go back to school or daycare?
If you or your child has gastro, it is important to stay home from work, school or daycare until the symptoms have been gone for at least 24 hours. Workers in childcare, the health industry and hospitality should not return to work for at least 48 hours after symptoms have gone.7,11,12
References
-
Elliot, EJ., 2007. Acute gastroenteritis in children. The British Medical Journal
-
Gastroenterological Society of Australia, 2010. Information about: Gastroenteritis in Children
-
Hand Hygiene Australia, 2018. Alcohol-based hand rub is the hand hygiene product of choice
-
Princess Margaret Hospital for Children, 2017. Emergency Department Guideline: Gastroenteritis
-
The Sydney Children’s Hospital, 2017. Fact Sheet: Gastroenteritis
This information is general and may not apply to you or another person. If you have any concerns about your health or the health and wellbeing of a child, consult a doctor or other healthcare professional. You should never delay seeking medical advice, disregard medical advice, or discontinue medical treatment because of information on this website.
← Back to blog
